ARDS
ARDS is also known as Adult Respiratory Distress Syndrome. The lungs can develop this problem during almost any type of critical illness.
Patients sick enough to be in the ICU undergo various biochemical reactions. These reactions cause the small blood vessels in the lung to develop leaks. The fluid portion of blood then accumulates in the lungs.
They become very congested, You can see the changes on the x rays shown below.
The fluid stiffens the lungs, making it very difficult to breathe. Patients try to compensate by breathing much faster; often twice the normal rate.
The extra fluid in the lungs also interferes with the ability to get enough oxygen into the blood. This means critical low oxygen levels being delivered all the tissues and vital organs.
Very low blood oxygen levels result in patients appearing dusky or bluish. This is easily seen around the lips and nail beds. It's known as cyanosis.

This is a chest x ray of a patient with ARDS
Any black areas are normal lung tissue.
The fluffy white areas are the congestion due to fluid collecting in the lung and air sacs.
These are responsible for preventing oxygen to get into the lungs and then out to the vital organs.
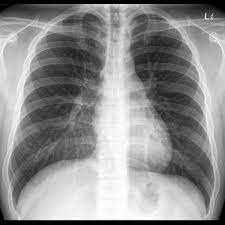
This is how a normal, healthy lung appears on an xray.
The black represents normal lung and filled with oxygen
The white triangular structure in the middle is the heart. It can barely be seen on the ARDS x ray above.
How Does ARDS Happen?
Any severe illness or sepsis can cause ARDS. The lungs seem to be a target for most of the types of problems that would require your loved one being in the ICU.
Septic shock may be the most frequent cause of ARDS. In this instance, the biochemical reactions mentioned above are most severe. Often tremendous amounts of fluid leak into the lung.
Direct injuries to the lung will also cause ARDS. These can include a direct contusion to the chest wall and lung, likely from a fall or auto accident.
Patients can vomit and large amounts of stomach fluid may flow directly into the lung, This fluid is usually very acid and can burn the lung tissue.
A direct lung infection or pneumonia, if severe enough can affect the entire lung and cause ARDS.
When the heart cannot effectively pump blood, such as in heart failure or after a severe heart attack, blood will leak up into the lungs. Another form of ARDS.
The table below lists the major causes adult respiratory syndrome.
Causes of ARDS
- Sepsis and Septic Shock
- Any Severe Illness
- Major Abdominal or Chest Surgery
- Multi Trauma
- Pneumonia
- Aspiration of Stomach Contents into the Lungs
- Pneumonia in Both Lungs
- Major Burns
- Heart Failure
What Actually Happens to the Lungs in ARDS?
The lungs have millions of tiny air sacs, also known as alveoli. They are surrounded or bathed by very small blood vessels or capillaries.
To keep it simple, in ARDS fluid leaks into the lung and eventually into the alveoli or air sacs.
This fluid causes two problems. First, it compresses the air sacs and they cannot fill with enough oxygen. Second the fluid can soon leak into the air sacs and prevent enough oxygen from entering.
The result of all this is low, life threatening oxygen levels. Patients compensate for the stiff lungs by breathing at a much faster rate that soon leads to fatigue.
Initial Treatment for ARDS
The biggest danger of ARDS is the low blood oxygen levels. This puts the brain, heart and other organs at serious risk of failure.
Oxygen levels need to immediately be increased to a safe range.
At the same time, the breathing rate must be slowed or total respiratory collapse might occur.
Short term, a face mask with 100% oxygen will be started. However this only buys some time. The fluid in the lung, causing all the trouble, must be dealt with.
The next step may be very high flow oxygen. Other choices include a very tight fitting face mask. This mask maintains higher pressures in the lung.
The high pressure increases the size of the compressed air sacs. This permits more oxygen into the lung. More oxygen can then enter the lung and ultimately be delivered to the vital organs.
When the situation is severe enough, a breathing tube may need to be placed. This allows connection to a ventilator. The ventilator can take over breathing, provide enough oxygen and expand the lung by applying continuous pressure.
Continued ARDS Treatment
For ARDS multiple interventions then begin. As mentioned, sepsis & septic shock are a major cause of this problem. The site of the severe infection must be identified and if able, removed by drainage or surgery. Powerful antibiotics need to be started.
Heart failure, causing back up of fluid into the lungs, must be treated. Diuretics will be given to rapidly eliminate the fluid.
Most of the other issues that cause the ARDS require symptomatic treatment. These include major surgery, trauma, burns , and strokes.
When ARDS Does Not Improve
When the above measures do not work or ARDS worsens, other, more aggressive therapies may be needed.
The ventilator will require adjustments of both pressure, the amount of oxygen delivered and it's breathing rate for your loved one.
Severe ARDS may require several weeks of ventilator support.
Some ICU doctors may decide to place the patient prone; for hours or days. This does not treat the ARDS ; but can improve the all important blood oxygen levels.
The patient below is on a ventilator and in the prone position. Depending on circumstances, this may be for several hours or days. It usually takes about four people, including nurses and respiratory therapists, to safely turn a patient.

The most severe, non responsive cases may require treatment known as ECMO or extra corporeal membrane oxygenation.
The patient is attached to a machine that temporally acts like an artificial lung. Blood is pumped from the patient while the ECMO device increases the oxygen level and lowers carbon dioxide.
ECMO may be necessary for one to two weeks.

An ECMO device at the bedside. The small size and portability means they can be used in transport around the hospital or from one hospital to another
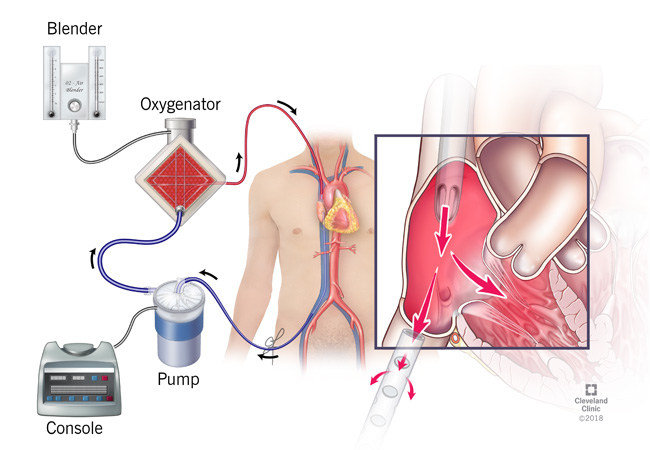
A schematic of an ECMO system. In this setup, blood (Blue) leaves the body and travels through a pump.
The oxygenator uses a blender to add the desired amount of oxygen.
The blood (Red) with increased oxygen, then returns to the patient
Other Therapies Necessary During ARDS
Patients on ventilators almost always require sedation. The ICU nurses continually adjust the amount to keep your loved one comfortable; but not completely unresponsive.
These medications also cause amnesia, Even though your family member may be responsive, he or she will fortunately not remember most of their ICU stay.
Other associated problems such as trauma, burns, or major surgery will require the addition of pain medications, also given continuously.
Ventilator treatment longer than seven to 10 days often means the need for a tracheostomy. A small surgical incision in the neck provides a route for the breathing tube .
Removal from the mouth is always more comfortable for patients. When the breathing tube is no longer needed it is removed at the bedside and the incision quickly closes.
Nutrition is extremely important in these very sick patients. They require large amounts of protein for healing and to prevent muscle breakdown and to fight infection.
A small soft tube is threaded through the nose into the stomach or small intestine. The specialized formula is delivered around the clock.
Recovery From ARDS
Survival and recovery from ARDS can be a slow process. The sicker the patient, the longer the recovery time.
The biggest hurdle, once the lungs recover involves gaining enough strength to completely breathe without the ventilator.
The combination of critical illness, prolonged bed rest, sedatives and the ventilator doing most of the work leads to very weak breathing muscles.
Just like any athlete, your loved one has to work daily to become strong enough to come off the ventilator. ICU doctors have various programs and exercises to make this happen.
The long term patients off benefit from short periods off the unit. Respiratory therapists and nurses can use small transport vents and monitors for this. The whole process provides much needed positive support for those frustrated with their progress.
Even before being completely off the ventilator, most ICUs will have patients starting with early walking.
In general, elderly patients will have a slower recovery, probably because of underlying chronic issues.
Questions to Ask
- What is the cause of the ARDS?
- Are the x rays showing improvement?
- Does excess fluid need to be removed?
- Can the sedation be reduced?
- Are antibiotics necessary?
- Will our loved one need a tracheostomy? If so, do you know for how long?
- Do you think our family member will need to be placed prone?
- When will you decide when to begin decreasing the ventilator support?
- How will we know if our loved one cannot survive?