- Home
- Broken neck
Broken Neck and the Need for the ICU
Most times a broken neck happens from major trauma. Automobiles and motorcycles account for the majority. Falls from a height are next.
The bones or vertebrae in the neck surround and protect the spinal cord. Severe trauma can fracture or displace these vertebrae.
When this happens the vertebrae then compress the spinal cord and cause the injury.
There are 7 vertebrae in the neck, Starting at the skull and going down, they are labeled Cervical 1-7 (C1-C7). Injuries above level C4 are always more serious.
The elderly can have loose neck ligaments leading to unstable vertebrae. Even in minor trauma, the bony parts can more easily move and compress and permanently injure the spinal cord.
Rupture of a disc in the cervical spine (neck) can also cause the injury. The disc slips out of place and causes the damage by compressing the spinal cord and leading to the injury.
A broken neck causes injury to the spinal cord and almost always causes some degree of permanent paralysis.
Most of the complications from a broken neck are severe enough to require ICU care.
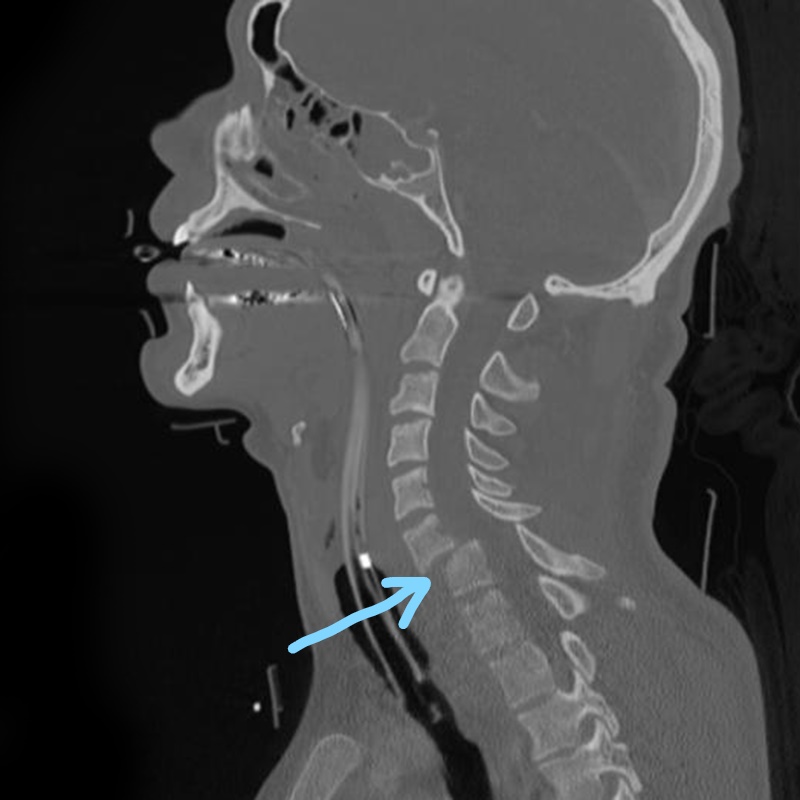
The arrow in this scan points to the injury. Here the vertebrae does not line up with the one above it, The displacement presses on the spinal cord and causes the injury.
Initial Treatment of a Spinal Cord Injury
When a broken neck is known or suspected, emergency personnel will place a stiff or hard neck collar on the victim. This prevents neck movement which otherwise could worsen the injury.
Also, before and after neck collar placement, the head will be held and stabilized to also limit any further movement.
Since a broken neck can cause low blood pressure and prevent normal breathing, these issues may need immediate treatment in the field by the EMT team.
An injury high enough in the neck to affect breathing, will require placement of a breathing tube prior to hospital arrival.
Treatment of low blood pressure, known as spinal shock, involves rapid infusion of intravenous fluids. Medications to increase the blood pressure will be continuously given along with the fluids.
Surgery is indicated if the vertebrae are displaced or directly compressing the spinal cord. This rarely improves the paralysis; does prevent further damage.
For some patients with a broken neck, the surgeon may first use neck traction. This helps to pull the vertebrae to better alignment and relieve pressure on the spinal cord.
Tongs are placed in the skull and weights applied to pull and straighten the neck. The doctors judge progress with repeat x rays of the neck.

A trauma patient in the field with a rigid cervical collar in place.
This prevents any neck movement which could cause further damage to the spinal cord.
Every time the injury moves higher up the spinal cord, the less the final recovery and a greater degree of paralysis.
The collar helps protect from worsening the injury.
Complications From a Broken Neck or Cervical Fracture
Paralysis
The spinal cord is very sensitive to any bruising or trauma. This causes swelling, which in turn increases pressure on the spinal cord itself. Permanent damage results.
This means severe weakness or paralysis. The higher up in the neck the injury, the more severe the symptoms.
There are 7 vertebrae in the neck; counting down from the base of the skull.
An injury at the mid level of the neck, cervical vertebrae 4 or above , will interfere with breathing muscles. A ventilator will usually be necessary. This means an ICU admission and a longer ICU stay.
A broken neck at a lower level of the spinal cord will affect arm, elbow, hand and finger function.
Low Blood Pressure
The nerves which control blood pressure to the rest of the body come from the spinal cord. Damage at the neck level, which is above those nerves, can lead to significantly low blood pressures.
This is known as "spinal shock" and will require continuously administered medications and intravenous fluids to stabilize blood pressure. These can only be given in the ICU.
Many times the blood pressure on it's own, after one or two weeks, will stabilize and medication can be stopped.
Pneumonia
Very likely, patients with a broken neck who require a ventilator will develop a pneumonia. Normally we keep our lungs clean and clear with coughs and deep breathes.
Those with a broken neck at cervical level 4 or higher cannot, on their own, cough or deep breathe.
Despite excellent work by the nursing staff to remove secretions; they can begin to pool deep in the lung. Many different hospital beds are available to help prevent the pooling of secretions.
The pooling will block airway passages and lead to infection. This is the definition of a pneumonia.
This type of pneumonia can be difficult to treat and may require multiple antibiotics and continuous suctioning and other aggressive techniques to keep the lungs clean.
It some cases, it may be necessary for the doctors to use a bronchoscope to clean up the lung.
This procedure enables the doctors to place the bronchoscope directly down into the lung. Sedation may be necessary.
They are then able to look through the device and move the tip to the specific lung areas that require clean up. Cultures can also be taken,
The cultures identify the specific bacteria present and help select the appropriate antibiotic.
In my own experience, these injuries can require bronchoscope use many times, as often as daily or every other day until things finally clear up.
Urinary Tract Infections
A broken neck can interfere with bladder and bowel function. During the first several weeks, a catheter in the bladder may be necessary to keep it drained and prevent pooling in the bed and macerating the skin.
Unfortunately, the catheter can serve as a two street and allow bacteria to travel into the bladder and infect the urine.
The doctors will continually look for and treat any sign of a urine tract infection. Untreated, the bacteria can lead to a serious infection known as septic shock.
Improvement of your loved one's condition allows removal of the catheter. It still necessary it can be placed several times during the day.
This method actually reduces the risk of infection. Since there is no longer any feeling in this area, there is no discomfort with the procedure.
Intestine Problems
Injury to the spinal cord will directly affect the stomach as well as the small and large intestines. They stop working altogether or slow way down.
This is especially so if the broken neck injury is high enough to require a ventilator.
Food or partially digested material cannot pass through. The stomach, large and small intestine all become distended.
The distention, if not treated, can increase the pressure on the wall of the bowel or stomach. A high enough pressure will cause rupture and spillage of contents into the abdominal cavity.
Several steps are taken to prevent this catastrophe. A tube can be threaded through your loved one's nose into the stomach. This continually drains stomach fluid to prevent any distention.
A second smaller tube is threaded into the small intestine(sometimes only into the stomach). A special fluid containing all the necessary nutrition is continuously dripped in at a slow rate.
The slow rate avoids any further distention. The fluid is designed to provide the correct amount of calories, protein, fats, and carbohydrates.
Skin Breakdown
A paralyzed patient cannot move him or herself. Continually laying in bed puts pressure on the coccyx or what we call the tailbone.
The skin can breakdown and become a non-healing wound; commonly called a decubitus. Breakdown can also occur on the back of the head.
The ICU nursing staff is primed to do everything to prevent this from happening. Your family member will be turned every 2 hours around the clock.
Special beds are utilized to help keep the patient from staying too long in any one position, These beds were described above in prevention of pneumonia.
If unfortunately a wound does develop, the nurses and physical therapists will do everything to keep it clean to help it heal. Most ICU's pride themselves in not letting a decubitus ever develop.
Depression and Communication Issues
As you might expect paralysis is a devastating and overwhelming injury. This alone will cause severe depression.
A ventilator make things even worse since now simple communication becomes very difficult. Lip reading or interpreting facial expressions causes much frustration to both your loved one and you.
Family visits along with anti depressants can help. Family members should be careful not to push their loved one so far that frustration develops.
It can be difficult to judge the level of depression even if you know your loved one very well.
Occupational therapists have many computers apps and devices to help with communication. Keep trying different ones until you find one that meets most of your loved one's and needs.
Favorite TV shows, movies and music all help. A head set will block out much of the disturbing noise common in many ICUs.
Below, is a type of rotating bed. It's designed to continually rotate. This prevent laying in one position, which will lead to skin breakdown and infection.

Blood Clots
Paralysis after a broken makes blood clots, usually in the legs a serious and possibly a life threatening situation.
Since the patient cannot move the legs or walk, blood will pool in the legs. The pooled blood can easily form clots.
After these clots form, parts can potentially break off and travel to the lungs. This is known as a pulmonary embolus.
The clots can reduce oxygen available to the lungs and seriously decrease blood pressure. Death can occur.
All paralyzed patients are given blood thinners. This greatly reduces the likelihood of any clots ever forming.
The physical therapists passively move the legs and arms to encourage blood flow and prevent any clots from developing.
Other Associated Injuries
The trauma which caused the broken neck and spinal cord injury often results in other severe and life threatening problems. These can include brain, chest and abdominal injuries.
All may require specific treatments and other surgical team involvements. Trips to the xray department, operating room and other areas may be necessary.
Care for your loved one can become very confusing as more doctors and others become involved.
The ICU Attending doctor will be aware of all that is happening and will keep you up to date as to how things are progressing and who is who.
When Can Our Loved One Leave the ICU?
Afte treatment for a broken neck and before discharge from the ICU, a number of problems need to be stabilized or resolved.
Ventilator
By the time of discharge, if still requiring the ventilator, your loved one will have a tracheostomy. The breathing is inserted through a small incision in the neck.
A tracheostomy is much more comfortable than the original breathing tube in the mouth. and can help in getting off the ventilator. New types of tubes can actually allow speaking on and off the ventilator.
After a broken neck, not all patients will come off the ventilator. The higher the injury above what's known as the C4-5 level, the less likely to be completely ventilator free.
The time off the ventilator could be during the day and on the machine at night. Other patients may be off only a few hours at a time. Some cases, with a high level injury may require round the clock ventilator support.
In all cases at this stage when ready to leave the ICU, the ventilator should only be necessary to assist with actual breathing. The lungs should require minimal or no extra oxygen.
After discharge most patients will go to a rehab or long term care facility. Going home on a ventilator is a complex issue and requires 24 hour care.
Diaphragm Help
Being able to stay off the ventilator for most of the day or night requires a strong diaphragm. This is the muscle which does most of the breathing work.
Spinal cord injury and the ventilator itself both cause the diaphragm to weaken. Help is available. Devices can now be surgically placed to help and strengthen the diaphragm.
When working properly, ventilator time can be reduced and in some cases eliminated.
Paralysis
Any paralysis, at the time of ICU discharge, will most likely be permanent. Any residual weakness can often be improved with intensive physical therapy.
Blood Pressure
By the time your loved one is ready to leave the ICU, any blood pressure issues should fixed. Some patients with high neck injuries may require a pill once or twice a day to keep the blood pressure in the desired range.
Intestine Problems
After a broken neck, two issues may prevent a normal diet. In some patients the tracheostomy can interfere with swallowing. Rehab and time can usually help fix this.
A second problem involves the stomach and intestines being very slow to return to normal function. Liquid tube feeds may still ne necessary.
For long term tube feeds, the tube is threaded through a small incision in the abdomen directly into the intestine. Then the tube in the nose can be removed with improved comfort.
Skin Breakdown
The paralyzed patient spends most of the time sitting in a chair or in bed. The prolonged time in either position can create enough pressure on the tailbone or buttocks to cause skin breakdown.
These areas need constant observation. Any indication of breakdown requires specific steps to relieve pressure on the affected area.
Nurses and physical therapists are a big help preventing and treating this problem. If the breakdown leads to infection, readmission to the hospital may be necessary.
Urinary Tract
Loss of bladder control can contribute to new urinary tract infections. Draining the bladder several times a day is very important. Signs of infection include fever and cloudy or foul smelling urine.
Depression
Obviously depression in the paralyzed patient will usually be present. Therapy and medication can help.
However in my experience, your loved one will do best and dramatically improve when in rehab and realize the other patients have the same problems.
Rehabilitation is a major step in getting your loved one back into a more normal and fulfilling life.
Re-learning daily activities and being able to do more on their own definitely improves the depression.
Questions to Ask
- What is the level of the injury?
- Will there be paralysis?
- Does are loved one know the severity of the injury?
- What should we tell our loved one about the injury?
- Will any of the paralysis improve?
- If so, how long will it take?
- If head tongs are used, are they helping?
- If surgery necessary, what result can we expect?
- Will surgery improve paralysis?
- Will our loved be able to return home?