- Home
- Heart Problems
- Heart Failure
Heart Failure
ICU Treatment
Heart failure has many different symptoms and causes. If severe enough or life threatening your loved on will require ICU care and treatment.
Failure means the heart has been damaged enough that it cannot pump the required amount of blood to the rest of the body.
Signs of Heart Failure
Fatigue, Shortness of Breath
Prior to ICU admission, a patient in heart failure will tire very easily.
If already in the hospital, simply getting out of bed, being bathed, or using the bathroom will wear him or her out.
Any activity will lead to shortness of breath, even to the point of being unable to speak.
You may notice this when the patient lies flat in bed, or even when fully upright.
Poor Vital Signs
Severe heart failure patients almost always have low blood pressure. Usually, a fast heart rate will try to compensate for the low blood pressure.
The heart rate may also be irregular. Oxygen levels will be low and shortness of breath is present.
Oxygen will need to be continuously administered.
Swelling
Since the heart cannot efficiently pump blood to vital organs, blood will back up.
This is noticeable in several ways. The legs may become very swollen and the abdomen distended as blood begins to collect in both places.
Neck veins become very prominent for the same reasons.
When any or all of these signs are present your loved one needs to be in the ICU.
How Does the ICU Team Diagnose Heart Failure?
Prior to movement to the ICU or after admission, the doctors' physical exams will confirm the findings described above.
A chest x ray will show lung congestion and often an enlarged heart.
An Echocardiogram uses an ultrasound probe on the chest wall to measure how well or poorly the heart is pumping blood.
It also measures the percentage of blood in the heart pumped out with each beat. This is a good measure of the severity of the heart failure.
If the percentage, known as the ejection fraction, is 20% or less, it indicates severe heart failure.
An electrocardiogram (EKG) will be done to look for irregular heart beat or other issues. It will be continuously shown on the bedside monitor.
The monitor will also show and record blood pressure, oxygen levels and any other values the doctors may want to continuously monitor.
If the heart failure is thought to caused by a blockage in a coronary artery, it may be necessary to take your loved one to the cath lab.
There, the doctors can inject dye and identify any severe blockage. If necessary, a stent can be placed to open up the blocked artery.
How Is Heart Failure Treated in the ICU
Anyone with heart failure severe enough to be in the ICU will need many things done immediately. Large intravenous catheters help deliver medications rapidly.
Fluid usually needs to be removed. A diuretic is a medication given to rapidly remove backed up fluid.
If the lungs are congested, very high flow oxygen or a tight fitting mask will be tried. If breathing is still difficult, then a tube will be placed through the mouth and into the lungs.
Your loved can then allow the ventilator to do the breathing and it will apply enough pressure to the lungs to improve oxygen levels.
Medications will be started to improve the heart's ability to contract and increase blood flow to all the vital organs.
It will probably be necessary to improve blood pressure by giving continuous medication intravenously.
New onset of an irregular heartbeat will also require treatment. Certain types may even require correction using an electric shock.
Your loved one will be sedated if this becomes necessary.
Special Mechanical Devices Used in Heart Failure
If the heart does not respond adequately to the various medications, mechanical devices are available until sufficient recovery has been made.
Implantable Cardioverter Defibrillator(ICD)
Patients in chromic heart failure and with a large heart are in constant danger of cardiac arrest. The internal defibrillator detects the dangerous irregular heart beat.
Placement of the device requires a minor surgical procedure. Sedation and local anesthesia will be given.
A small controller box and battery are placed under the skin; usually just below the collar bone. Leads are attached to the box and threaded to the heart.
When a life threatening, irregular heart beat is detected the device immediately sends an electrical shock to stop the threatening heart rhythm and return to a safe heart rate and rhythm.
This is a permanently placed device. Your loved one will go home with it. Regular check ups monitor how well it's working and when the battery needs to be changed.
ECMO
The full name is extra corporeal membrane oxygenation. ECMO requires large catheters usually placed in the groin or neck.
It runs continuously and ensures that adequate blood and oxygen get to the vital organs. This allows time for the heart to begin healing.
The device may be required for up to 2 weeks. The patient will be in the ICU the entire time.
Since the blood needs to be thinned to prevent clotting in the lines going to and from the machine, bleeding can occur. This can causes new problems if the bleed is in the brain.
In addition to the ICU team, an ECMO team monitors your loved the entire time the device is needed.
The goal is for the heart to improve enough to take over completely and pump enough blood tp allow the ECMO to be stopped.
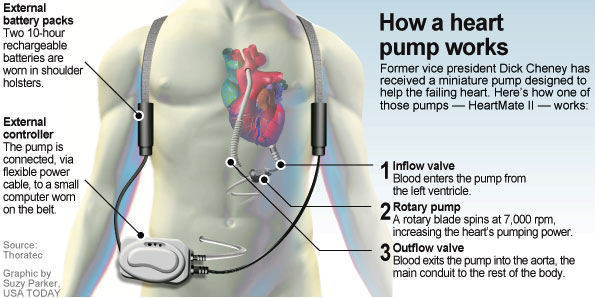
Ventricular Assist Device(VAD)
This device requires an operation. Once in place it provides most of the blood pumping for the heart. These devices are now small enough to be portable.
When all other problems are fixed or stabilized, your loved one can be discharged from the ICU and eventually go back home.
Usually the VAD is placed when the heart is not expected to recover or improve. In many cases the patient is waiting for transplantation and a new heart.
If a transplant is not possible, the VAD becomes a permanent device. Once stable, the patient can then leave the hospital.
At home. constant monitoring checks on battery life and how well the device is working.
Complications in and out of the ICU include the device clotting and stroke or bleeding in the brain.
Below is an illustration of a ventricular assist device
Questions to Ask
- What caused the heart failure?
- Will it happen again?
- Can the heart failure be prevented?
- How long will our loved one be in the ICU?
- Are other organs involved or injured?
- Will the ICD prevent heart failure?
- If the ICD goes off and shocks our loved one, what should we do?
- Will the VAD be permanent?
- Will a heart transplant be needed?
- Can our loved one go home on ECMO?
- What happens if there is a brain bleed or stroke?
- What should we do if the kidneys fail?
- How long will the ventilator be necessary?