- Home
- Traumatic Brain Injury
- Ventilator
Ventilator Use in the ICU
In the ICU a ventilator will be used for several different problems or complications.
The machines do not really cure anything. They merely stabilize your loved one's lungs until they can heal and recover.
The ventilator also ensures adequate oxygen and carbon dioxide levels and eases breathing efforts.
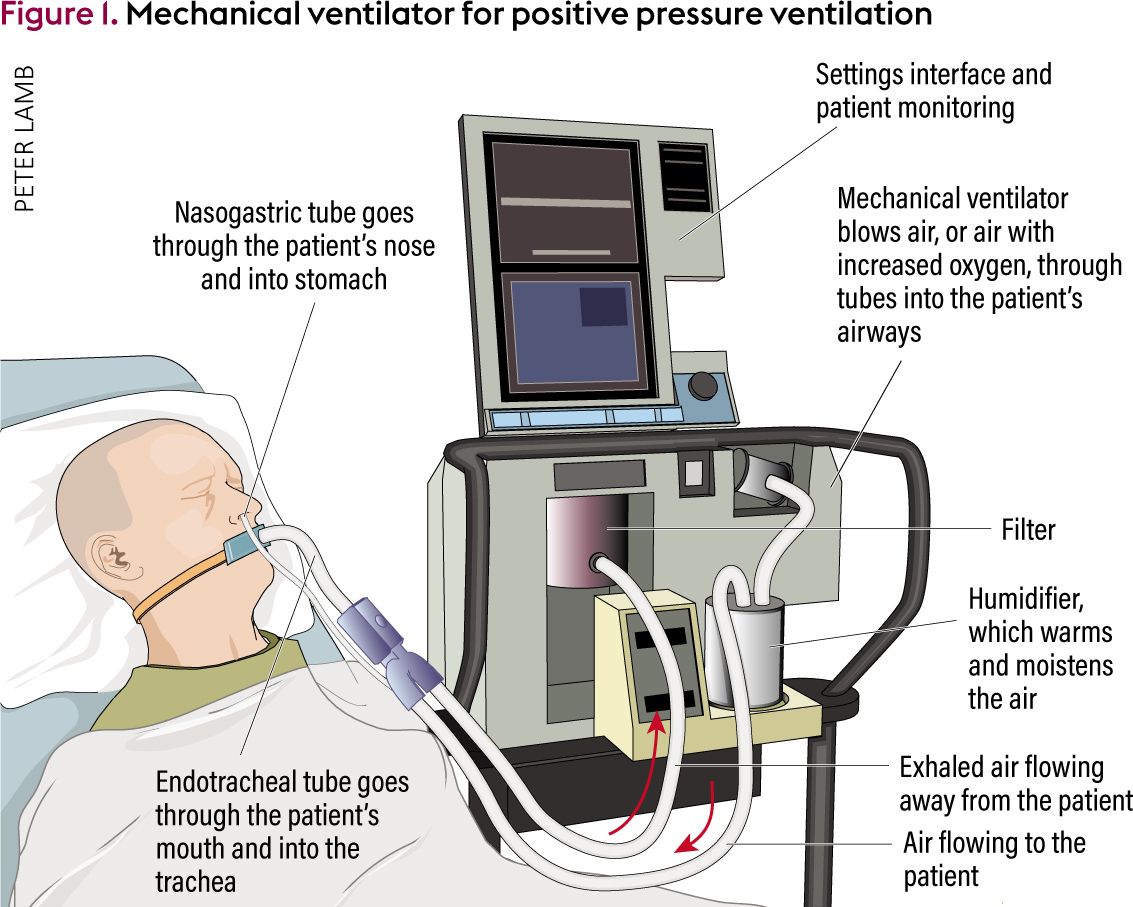
We have many different types of ventilators. The picture below points out in general all the necessary parts.
Conditions Requiring a Ventilator
After major chest, heart or abdominal surgery, keeping a patient on a ventilator overnight allows use of enough pain medication and sedation without the worry of depressing the patient's breathing.
Very sick patients can retain fluid in the lungs. This causes severe congestion. The patient has difficulty breathing and develops very low blood oxygen levels.
This congestion is known as Adult Respiratory Distress Syndrome(ARDS) or Acute Respiratory Failure(ARF).
The condition develop because from problems such as massive sepsis, bilateral pneumonia(both lungs), or severe heart failure.
The ventilator provides enough oxygen and also eases breathing. Without the ventilator in these situations, survival is not possible.
Patients with severe, chronic pulmonary disease(COPD) can deteriorate and require a ventilator.
The ventilator primarily keep their carbon dioxide levels in an acceptable range and assist with their breathing.
Other Conditions
Patients comatose from a large stroke do not breathe well on their own. The ventilator assures adequate breathing and helps keep the lungs clear.
Ventilators are used when airway protection is necessary. Surgery or injuries to the back of the throat or neck can cause swelling and block air getting to the lungs..
A breathing tube is placed to bypass the swelling or blockage. When connected to a ventilator the patient can easily breathe.
This also permits adequate pain control and sedation.
Caring for a Ventilated Patient

Above,a breathing or endotracheal tube that is placed through a patient's mouth.
The ventilator itself is not uncomfortable; the breathing tube can be.
Patient usually require at least mild sedation.
After surgery or trauma pain medications will also be needed.
Since your loved one cannot talk with the breathing tube in place, he or she can become very frustrated. Lip reading or writing messages are usually not satisfactory.
Patients often report that while they were on the ventilator, suctioning was painful.
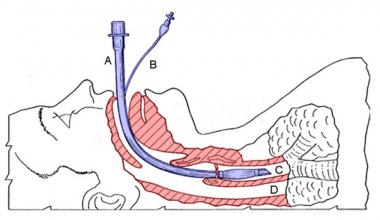
Below is a breathing tube through the mouth and directed towards the lung - Fig C. Fig.D is the esophagus leading into the stomach.
Medical Ventilator Management
In most ICUs a chest x ray every day helps judge how the lungs are doing.
Ventilator changes are made after x rays and blood tests. Finger tip the breathing tube probes give continuous oxygen and carbon dioxide levels.
Ventilator adjustments or changes are based on all this information.
If pneumonia is possible, the doctors place a small scope through the breathing into the lungs to obtain a culture and clean out secretions.
We call this a bronchoscopy. Extra sedation will be required for the procedure which takes about 15-20 minutes.
Tracheostomy
In most ICUs if a ventilator is expected to be needed for 5 or more days, a tracheostomy may be done

A tracheostomy tube. Shorter than a breathing tube. Placed through a neck incision.
Usually at the bedside with anesthesia, the surgeon makes a small incision in the neck. A tube is placed into the patient's airway(trachea).
The tracheosotmy tube is attached to the ventilator and the tube in the mouth removed.
This is more comfortable for your loved one. When no longer needed, the tracheostomy tube is simply removed without another procedure needed.
Below is a an illustration of a tracheostomy tube in place. It does not pass through the vocal cords. After ventilator removal, it may stay in place for a number of days.
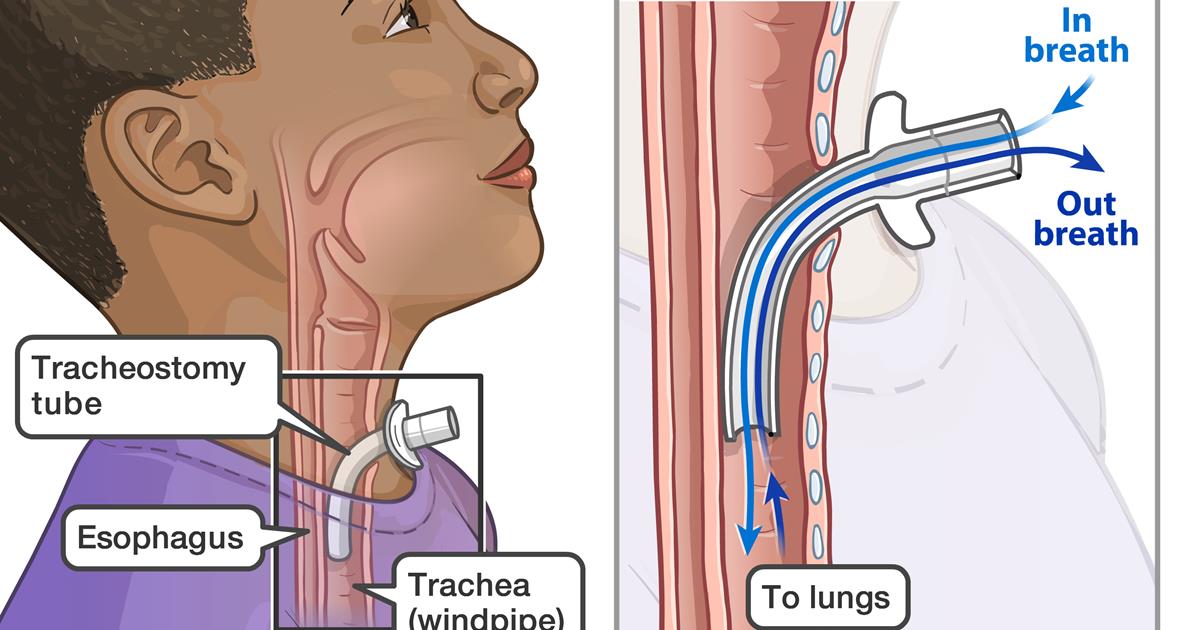
Tracheostomy also prevents vocal cord damage. The tube through the mouth passes through and continually and irritates the vocal cords.
After several days it can cause injury. The tracheostomy tube is placed below the vocal cords.
Ventilator Removal
If the ventilator was only used overnight after elective surgery, it can easily be stopped and removed the next day.
For other patients, the time on the ventilator will depend on how sick they are and how fast they are recovering.
While on the ventilator, a patient's breathing muscles weaken. As your loved one improves, it may take several days before he or she is strong enough to remove the ventilator.
This is known as weaning. It usually involves the patient breathing more on their own each day and reducing oxygen from the ventilator.
When the patient is stable and strong enough, the ventilator is removed.
Talking after the tube removal, while possible, may at first be difficult due to hoarseness. This usually clears up in 1-3 days.
Questions to Ask
- Why can't our loved one talk while on the ventilator?
- How do you decide when to take out the breathing tube?
- What does it mean to"wean the ventilator"?
- Is sedation necessary while on the ventilator?
- I was told once on the ventilator, a patient will never come off
- Can our loved get out of bed or leave the room while on the ventilator?
- How does a patient eat when on the ventilator?
- Why is a tracheostomy needed?
- How long will the ventilator be needed?
- Can a patient go home on the ventilator?
- What does the respiratory therapist do?
- Can our loved one be transferred to another hospital while on the ventilator?